As Biolabs Multiply, Concerns About Oversight Grow
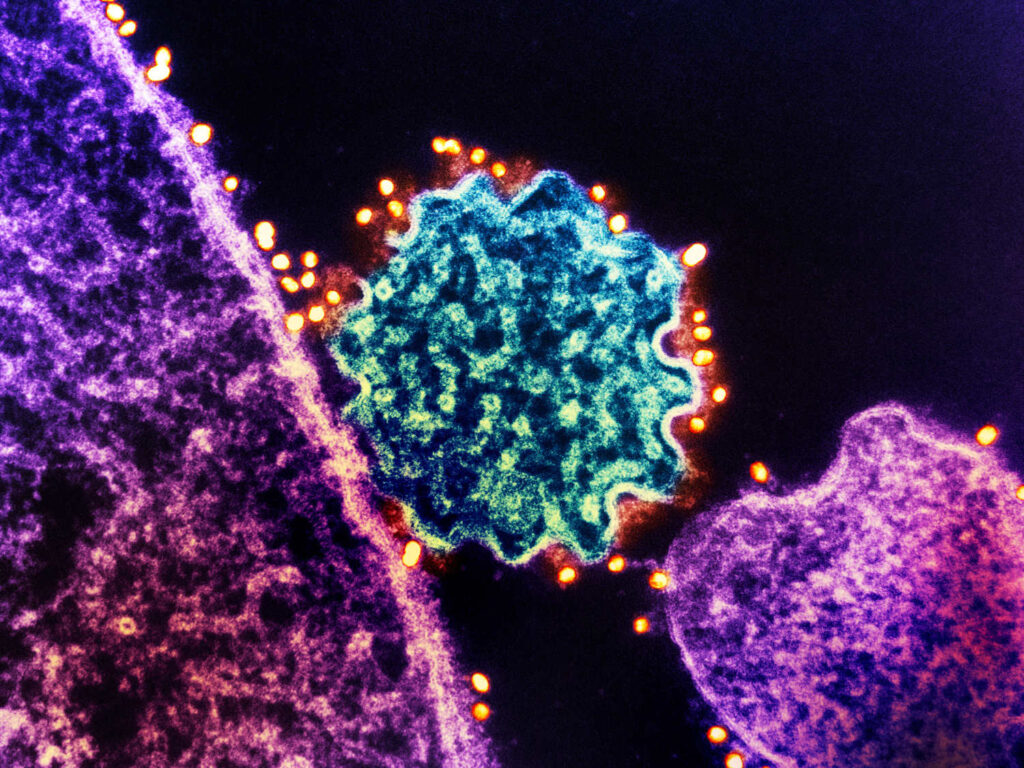
India’s policymakers have ambitious plans for pathogen research. Can safety infrastructure keep up? A researcher works in a specialized Class II cabinet in a BSL-3 lab in Hyderabad, India. (Taniya Sarkar for Undark)
A researcher works in a specialized Class II cabinet in a BSL-3 lab in Hyderabad, India. (Taniya Sarkar for Undark)
Raghunand Tirumalai loves to talk about how well-run his laboratory is. “We’re very proud of the setup we have here,” he said on a Friday afternoon in October, standing in his office on the campus of the Center for Cellular and Molecular Biology (CCMB) in Hyderabad, India. The office was decorated with colorful artwork, including posters about tuberculosis and tiny plastic figurines of deadly bacteria and viruses.
Tirumalai joined CCMB in 2008 to study what makes the tuberculosis bacterium so virulent — knowledge that can help design better treatments for a disease that kills tens of thousands of people in India every year. This requires his team to work with live tuberculosis bacteria, a high-stakes dance that takes place under rigorous safety protections.
To enter the lab, Tirumalai first scans his fingerprint at the door. Next, he passes through two change rooms. In the first, he puts on shoe covers, a hair net and latex gloves. He also dons a puncture-resistant Tyvek suit, an N95 mask and safety goggles. In the second room, he snaps a second pair of latex gloves onto the cuffs of his suit so that no skin is exposed.
Inside the final door, the fluorescent-lit room has crack-free walls, gleaming steel tables and smooth epoxy floors so no pathogens can escape a scrubbing. The air cycles through HEPA filters. To minimize infection risk, researchers handle pathogens inside Class II cabinets, large glass-fronted boxes.
In a room above the laboratory, large machines pump day and night to keep the air inside at a lower pressure than the surrounding building, so airborne pathogens won’t flow out of the room.
No single authority oversees high-containment labs around the world.
Facilities like CCMB’s are crucial for pathogen research. They are also at the center of ongoing debates over how to balance the need for lab space with the risks of handling — and sometimes re-engineering — pathogens.
High-containment facilities around the world work with such pathogens. No single authority oversees these labs; no single treaty governs them or ensures high standards; nobody is even sure how many there are. In some countries, the labs are tightly regulated, at least on paper; in others, they are not.
Some pathogens and experiments pose broad risks, and even intensive safety protocols can fail. One recent analysis of the global scientific literature identified 94 incidents of lab leaks between 2000 and 2021, infecting 309 people and killing eight. Some experts believe that kind of leak, at a lab in China, was responsible for the COVID-19 pandemic. Although many other experts strongly disagree with this take, subsequent investigations have uncovered safety lapses at Chinese labs and set off fierce debates about how to oversee risky research worldwide — especially for those rare experiments where a major breach could have global consequences.

At the same time, the pandemic has also prompted what some experts describe as a global boom in the construction of such facilities. As countries struggled to respond to the pandemic, many decided that they need more laboratories to prepare for future outbreaks.
Those tensions are apparent in India, the world’s most populous nation and a global biotechnology powerhouse. According to the Department of Biotechnology, the country has 47 certified research laboratories (including the CCMB facility in Hyderabad) rated to biosafety level 3, meaning they allow scientists to work with highly transmissible pathogens like coronaviruses or West Nile virus — more than almost any other country in the world (although far behind the U.S. and probably China). India also has one functional facility rated at the highest biosafety level, BSL-4, meaning they can work with lethal pathogens that have no known cure. (Another was reportedly inaugurated in November 2024.)
More may be coming: After the first waves of COVID-19, state and national officials in India announced ambitious plans to expand pathogen research. Since then, proposals to build at least 26 new BSL-3 and at least four new BSL-4 laboratories have been announced. More vaccine manufacturing facilities that work with live viruses are also under development — although it’s not clear regulators even know how many of those facilities exist in the country.
Can safety infrastructure keep up with ambitious plans for pathogen research?
Policymakers introduced new biosafety regulations in 2017, but interviews with more than two dozen scientists and biosafety experts suggest that implementation is ongoing. Some key government labs have practices on par with international standards, but many others are yet to catch up. The country has a shortage of biosafety professionals, several experts said, and there’s sometimes limited awareness of safety protocols: In many labs, “my sense is that the scientists don’t really fully understand why it’s important,” said Shruti Sharma, a fellow at Carnegie India who has studied pathogen research in the country.
Meanwhile, even regulators seem to be uncertain about who — if anyone — within the government is responsible for monitoring biosafety protocols at vaccine manufacturing facilities.
The impact of these gaps is hard to judge, given that Indian regulators are opaque with key data, such as the numbers of biosafety accidents. As such, there remains some disagreement over whether the growth of BSL-3 and BSL-4 laboratories here represents a global threat, and some Indian scientists at key government labs argue that concerns are overblown.
India has far fewer high-containment laboratories than the United States, which has experienced its own share of laboratory safety issues. And researchers in India — as in other countries in the Global South — appear to be working mostly with pathogens that circulate widely outside laboratory walls. They tend not to perform the kind of research, sometimes called gain-of-function research of concern, which aims to deliberately make pathogens more deadly or more transmissible, and that can provoke intense controversy.
What’s clear is that India’s policymakers have ambitious plans for pathogen research. Can safety infrastructure keep up?
* * *
It’s not always easy to work with viruses and bacteria without getting infected by them, and building and running a high-containment lab is difficult and expensive. In Hyderabad, the roughly 500-square foot CCMB facility cost around 20 million rupees (around $235,000) when it was built in 2010. Lab workers must get certified before they can enter the lab, and an engineering team needs to be available in case the equipment malfunctions.
A BSL-4 lab is even more complex. The facilities are “a beast” to run, said Chandrabhas Narayana, the director of Kerala’s Rajiv Gandhi Center for Biotechnology. A BSL-4 lab must be either housed in its own designated building or isolated in a restricted zone of a building, and policies to sterilize waste are more stringent than for BSL-3 facilities. Lab workers must change clothes before entry and shower before exit, instead of just putting on masks and suits. The biosafety cabinets are airtight, and when scientists are handling pathogens outside them, they must wear positive-pressure suits, which resemble spacesuits.
With each new safety feature, the costs escalate. In 2020, the Rajiv Gandhi Center planned to build a 10,000 square foot BSL-4 lab. Such a facility would have cost an estimated 1 billion rupees (around $11.7 million) to set up, and an additional 500 million rupees each year to operate, according to Narayana. (Ultimately, the proposed BSL-4 lab wasn’t built.)

Since the early 2000s, more countries have decided those expenses are worth taking on. The Indian government opened the first BSL-4 laboratory in Asia in 2000 at the National Institute of High-Security Animal Diseases, or NIHSAD, which works on veterinary pathogens such as avian influenza. The next decade also saw the construction of several government-funded BSL-3 facilities, many working with tuberculosis. At the time, India had a skeletal biosafety framework, that was geared heavily toward genetic-engineered plants. So, scientists involved in building these early labs relied on biosafety guides from the World Health Organization and the U.S. Centers for Disease Control and Prevention to develop their own protocols, said Harshad Murugkar, biosafety officer at NIHSAD.
The published literature suggests that biosafety at some Indian research labs was deficient. A 2002 paper, for instance, linked two polio outbreaks in the country to one or more lab leaks.
More BSL-3 labs were constructed in the 2010s, along with the National Institute of Virology’s BSL-4 facility in Pune. But by then, the NIHSAD decided to re-classify itself as a BSL-3, given the high costs of upkeep and the increasingly stringent global standards for the highest-security labs.
It’s unclear when the first Indian BSL-3 vaccine manufacturing facilities were built, although at least two companies claim to run them today.
As high-containment laboratories opened in India and other countries, experts raised concerns about biosafety practices in the Global South. Around 2012, anonymized inspections co-sponsored by the Asia-Pacific Biosafety Association in multiple Asian countries found widespread issues.
Around that time, experts at the U.S. National Academies of Sciences conducted multiple workshops on laboratory safety, repeatedly identifying deficiencies in laboratories in South and Southeast Asia. At one 2014 meeting sponsored by the organization, Aparna Singh Shah, a World Health Organization official stationed in New Delhi, described laboratories in the region as poorly monitored, underequipped and staffed by workers with little training, according to a summary of her remarks. “Biosafety and biosecurity awareness and practices are inadequate,” the summary warns.
* * *
In 2014, around the time of the National Academies of Sciences meetings, experts in the U.S. were undergoing their own reckoning on biosafety, after a string of missteps at government labs. And more critics were wrestling with that fact that, for all the high consequences of pathogen research, regulation around the world was often sparse — or didn’t exist at all.
Many countries today oversee pathogen research using a model developed in the U.S. in the 1970s, which permits research institutions working with dangerous pathogens to largely police themselves. Even today, some pathogen experiments in the U.S. are unregulated, or bound only by a set of guidelines, also originating in the 1970s, that allow scientific institutions and their government funders to proceed with limited independent oversight.
Even today, some pathogen experiments in the U.S. are unregulated.
As was the case in many countries, Indian regulations, which debuted in 1989, took their cue from the American model. They left most lab oversight to local committees of scientists, called Institutional Biosafety Committees (abbreviated in India as IBSCs), who reported to a national committee of expert scientists.
“Even as recently as 10 years ago, there still was no national framework for what biosafety should look like in the tens of thousands of clinical and diagnostic and research labs and pharma across the country, and that was a bit surprising,” said Ryan Burnette, a biosafety and biosecurity expert at Merrick and Company, an engineering firm, who has consulted on laboratory construction and maintenance projects in India. “They were well behind the curve a decade ago, and I think they’re still slow to catch up on that.”
Indian regulators were aware of such concerns, said SR Rao, a senior official in the Department of Biotechnology who retired in 2019. Overseas visitors often complained about glaring biosafety shortcomings, worrying policymakers. “There was a serious concern in higher offices,” Rao said.
In 2017, Rao’s office revised the country’s biosafety rules. Under a new certification system, BSL-3 labs have to get a certified external agency to test all their equipment each year.
The new regulations, and a series of awareness programs that government officials conducted subsequently, led to changes at some facilities. Many labs that had not formed IBSCs did so after 2017. In Mumbai, a nonprofit lab doing tuberculosis research had to extensively rework the building for their BSL-3 facility after scientists there realized their old plan wasn’t in line with regulatory requirements.
But even as the new rules went into effect, the country had to grapple with another problem: It didn’t have enough laboratories to deal with a crisis.
* * *
When COVID-19 hit India, researchers there found themselves desperately short of laboratory space to study the virus. The onus of drug testing and research for a country of more than 1.4 billion people fell on India’s few dozen BSL-3 labs.
“That’s when we woke up and said, look, if this happens to us again, then we have no way of handling it,” said Tirumalai, from CCMB. “The load is going to be too much for one institute.”
Even before COVID-19, researchers said, a shortage of laboratory capacity could make it hard for them to deal with emerging threats. For instance, public health researchers in the state of Kerala, which experiences outbreaks of deadly Nipah virus every few years, have to rely, for some research, on the BSL-4 laboratory in Pune, over 800 miles away. The shortage of laboratory space delays important science: Narayana, of the Rajiv Gandhi Center in Kerala, said their institute helped developed an antibody treatment for the Nipah virus, but is waiting to test the treatment in animals at the Pune facility.

During the pandemic, policymakers rolled out plans to build more labs. In 2021, the Indian government’s annual budget included plans for nine new BSL-3 laboratories as part of a scheme to build new health infrastructure. Two years later, the health ministry disclosed plans for two BSL-4 and four BSL-3 mobile labs as part of the same scheme. Additionally, the National Center for Disease Control was to get its own BSL-4 lab and 11 new BSL-3 labs.
Separate from these programs, in November 2024, the Defense Research and Development Establishment (DRDE) announced the opening of a BSL-4 facility in the central Indian city of Gwalior, intended to focus on early outbreak detection in India. That brings the number of the highest level of existing biosafety labs in the country to two. DRDE did not respond to Undark’s request for comment.
States are planning their own facilities, too. Kerala’s Institute of Advanced Virology has already picked a location for its own BSL-3. A BSL-4 is also in the pipeline, said Eswaran Sreekumar, director of the institute, although the timeline is not clear. Sreekumar said that the Kerala government wanted its own research facilities, given that the state has seen outbreaks from many zoonotic pathogens, including Nipah and West Nile virus.

In Gujarat, the state government has designated 2.2 billion rupees (around $26.4 million) to construct a complex containing BSL-2, BSL-3 and BSL-4 labs to research pathogens such as Crimean-Congo hemorrhagic fever virus, which has caused outbreaks in the state.
It’s not clear if all these plans will come to fruition. If they do, they would leave India with at least seven BSL-4 laboratories, among the largest number in the world, and more than China probably has today.
* * *
Overseas, biosafety experts in the U.S. and other countries in the Global North have sometimes greeted those kinds of expansions with a mix of welcome and alarm.
For years, the U.S. government — through agencies such as the U.S. Centers for Disease Control and Prevention and the Defense Threat Reduction Agency — has helped to advise the construction of high-containment laboratories around the world.
At times, though, the global growth of high-containment laboratory capacity has also prompted concern.
Last year, an investigation in the Washington Post described how “governments and private researchers continue building high-containment laboratories to work with the most menacing pathogens, despite a lack of safety standards or regulatory authorities in some countries.”
“There’s always room for improvement both here at home and abroad.”
In 2023, the Global Biolabs project, an influential collaboration between academic institutions in the U.S. and U.K., raised concerns about “the global boom in construction of BSL-4 and BSL-3+ labs, particularly where biorisk management oversight is weak.” The report singled out India for having ambitious plans for laboratory growth, while assigning the country low scores on governance, biosafety and laboratory security policies. (The report, seemingly in error, describes India as lacking biosafety legislation.)
In interviews, biosafety experts who have done work in the country say there’s a strong commitment to biosafety in top institutions — but also persistent issues with implementation.
“I don’t want it to sound like I’m casting India, the U.S. or any other country’s biosafety/biosecurity practices in a negative light, because that’s not the case,” wrote Antony Schwartz, an Indian American biosafety expert, in an email to Undark. “The vast majority of research is being conducted safely,” he added, noting that “there’s always room for improvement both here at home and abroad.”
Schwartz began visiting India in 2023 on U.S.-government-funded trips to help train scientists on biosafety protocols. (In his day job, Schwartz is the top biosafety officer at Duke University; he spoke with Undark outside that capacity.) The rules on paper, he said, are promising. “But is it followed consistently, or is it moving at a pace that is equivalent to other places? Not really,” he added.
Those issues start in individual labs, where researchers may be unaware of biosafety issues, several experts said. Safety and security are sometimes treated as an afterthought, said Aparupa Sengupta, a global biosafety and biosecurity expert. Unlike in the U.S. and Europe, laboratories rarely have full-time officers dedicated solely to biosafety, she noted. Instead, the person responsible for preventing a leak is often handling biosafety on top of another job, sometimes with limited training. “They also have to publish, and they also have to present, and they also have to manage people, and they also have to do biosafety,” said Sengupta, who works as senior program officer at the Nuclear Threat Initiative.
Another problem, some experts said, is a shortage of good Indian training programs for biosafety professionals. One of the risks as India builds more BSL-3 and BSL-4 labs, Murugkar said, is that there won’t be enough experts to run them.
There’s limited professional support for those tasked with biosafety. Many other countries in the Asia-Pacific region have a national professional association for biosafety. But an organization founded in India in 2008 by NIHSAD scientists fizzled within a few years. (Efforts are underway to restart the organization, Murugkar said.)
“I feel like on the biosecurity front, India is largely still very much the Wild West.”
The new regulations, experts said, also have some gaps. One such area is the lack of biosecurity policy, referring to measures that aim to prevent intentional misuse of pathogen labs and research — such as by someone wishing to create a bioweapon. In the U.S., for example, people must register with the federal government and pass background checks before they can access certain pathogens. Few nationwide rules in India govern who can work with dangerous pathogens.
“I feel like on the biosecurity front, India is largely still very much the Wild West,” said Burnette, the consultant.
At the national level, current and former members of the Review Committee on Genetic Manipulation (RCGM), the chief biosafety regulator to whom the IBSCs report, maintained that Indian regulation had kept up with the expansion of high biocontainment labs in India. “We are moving in the right direction,” said Vinay Nandicoori, a current RCGM member and the director of CCMB in Hyderabad.
And the institutional biosafety committees, provide rigorous oversight, said Tirumalai, who is a member of five IBSCs, including CCMB. Each IBSC has a government nominated member, and its composition is approved by the central regulator. They take their jobs seriously, Tirumalai said, going over every detail in proposals: “There’s no messing around.”
But, in interviews with Undark, some current or former members of RCGM said that the group’s powers of oversight over institutional biosafety committees were limited. The core committee consists of around 20 expert scientists, according to meeting minutes, supported by a small team of full-time staff. The team has other responsibilities, including oversight of genetically modified crops. Lab biosafety is “a very small part of” the committee’s job, said Amita Aggarwal, who was an RCGM member until 2022.

If IBSCs don’t function as they should, the RCGM is limited in what it can do. “RCGM cannot check the entire country,” said Rakesh Mishra, who served as chairman of the committee. So, the committee’s policy has been to train IBSCs, and inculcate the importance of biosafety.
A lot can escape the radar of such a regulatory system, such as research accidents. Some countries, including the U.S., have systems to report minor lab incidents, such as when a person working in a lab accidentally spills a small amount of culture, but isn’t infected. Such incidents serve, in theory, as an early warning system of problems in a laboratory, although they rely on individual scientists and biosafety committees to be forthcoming about their mistakes.
In India, multiple researchers interviewed by Undark said they did not report minor accidents to the RCGM, and that these were handled internally by the lab and IBSC. And Mishra, the central regulator’s former chairman, said that even though Indian labs were required to have strong internal reporting and record-keeping systems, that was often not the case in practice.
RCGM doesn’t share the numbers or details of the accidents that get reported to it, either. The body declined requests under India’s public records law about the number of research accidents reported in the past six years, citing an exemption for information that prejudicially affects the “security, strategic, scientific or economic interests of the State.”
The laboratories working with the highest security protocols, India’s BSL-4 labs, may not be reporting routinely to RCGM at all. In interviews, current and former members of RCGM said they did not know whether it was part of their mandate to review activities at the National Institute of Virology (NIV) and the just-established BSL-4 lab at the DRDE. Nitin Jain, a member of the RCGM, said his team does not yet have a certification program in place for BSL-4 labs. (NIV leaders did not respond to interview requests from Undark.)
“All regulatory regimes in India are very soft and therefore potentially corrupt.”
It’s also unclear who is overseeing biosafety practices in India’s large vaccine manufacturing industry. At least two vaccine manufacturers claim to have BSL-3 facilities where they manufacture an inactivated SARS-CoV-2 vaccine and a vaccine for foot and mouth disease, which only affects animals. India also plans to build facilities for manufacturing vaccines against poliovirus, which are required to follow high biosafety standards, comparable in stringency to BSL-3 facilities.
Biosafety at such manufacturing facilities is a whole different ballgame compared to research labs, said Raman Rao, CEO at the Singapore-based Hilleman Laboratories, a vaccine research firm. Vaccine manufacturing plants handle far larger amounts of live virus at a time, compared to research labs, Rao said, and are typically regulated by the country’s drug regulator, rather than a research regulator like RCGM. But in India, the regulatory system is unclear. RCGM’s Jain said regulation of vaccine manufacturing doesn’t fall under the committee’s purview. And in response to a public records request from Undark, that regulator, the Central Drugs Standard Control Organization (CDSCO), said it had no data on how many manufacturing facilities in India are certified as BSL-3.
CDSCO director Rajeev Raghuvanshi did not respond to a list of questions from Undark.
Weak regulation is a theme that runs across many sectors in India, making it a concern for biosafety too, said Satyajit Rath, an immunologist who has served on biosafety committees in India. “This is not to do with science. It’s not to do with biosafety. Even the drug regulatory regime, revenue governance regulatory regimes, all regulatory regimes in India, are very soft and therefore potentially corrupt in coercive, selective fashion,” he said. “That’s the basic fact of life that all of us deal with every day.”
* * *
Does pathogen research in India pose widespread risk? After all, lab leaks typically harm laboratory workers, and perhaps their close contacts, but spread no further. And many laboratories in the Global South are working simply to track pathogens circulating in the wild — not to conduct the kind of higher-risk gain-of-function experiments that have been the subject of recent scrutiny.
Some experts invoke the example of China, which announced plans to construct a network of high-containment laboratories in 2004, after the SARS outbreak. By the end of 2013, China had 42 BSL-3 laboratories, with its first BSL-4 under construction in Wuhan.
The network, according to papers by Chinese academics, was designed to track and respond to outbreaks. By the late 2010s, though, researchers were performing higher-risk work with the help of U.S. funding, including manipulating coronaviruses at the country’s flagship BSL-4 facility, the Wuhan Institute of Virology (WIV).
Experts disagree over whether this work may have accidentally sparked the COVID-19 pandemic. But there’s some evidence that biosafety practices in China were deficient. A 2019 paper by WIV’s National Biosafety Laboratory director described funding shortfalls at many laboratories, as well as a national shortage of dedicated biosafety experts that made it “difficult to identify and mitigate potential safety hazards.” A recent report from Republicans in the U.S. Senate describes persistent safety lapses at WIV, including equipment failures and decisions to conduct work on SARS coronaviruses outside high-containment laboratory spaces.
The revelations have revived longstanding critiques of pathogen research.
There’s some evidence that biosafety practices in China were deficient ahead of the outbreak of COVID-19.
Richard Ebright, a molecular biologist at Rutgers University, organized efforts to oppose the expansion of high-containment laboratories in the U.S. in the early 2000s.
Proponents said the new laboratories would help the country respond to pandemics and bioterrorism. But Ebright was unconvinced. The boom in new laboratories, he warned, raised the odds that a pathogen would accidentally escape. And it expanded the number of people who had the tools to commit acts of bioterrorism. “We believe that increasing the number of institutions and people with access to bioweapons agents will increase the likelihood of their release,” he and a colleague wrote in a 2002 correspondence to the journal Nature.
Today, Ebright looks askance at the growth of such facilities worldwide. “The historical pattern is that the expansion of high-level biocontainment capacity comes first,” he said in a recent conversation with Undark. “After the facilities are built, they are empty white elephants.” In order to justify the costs, Ebright continued, scientists find projects to perform there, which can push them toward research that involves engineering pathogens. “If the nation has one BSL-4, and is planning two additional ones, that nation predictably will be doing high-risk research at BSL-4 to justify the construction decision and the continuing operational cost decision.”
Ebright discussed both China and the U.S. as examples of places where expansions of BSL-3 and BSL-4 capacity were followed by scientific experiments that alarmed some outside observers and scientists. “It happened,” he said, “each place new BSL-4s have gone up.”
Not everyone shares those concerns. Many researchers in India say the work conducted in their laboratories is not especially high risk — and some say that, unlike in the U.S. and China, there are few incentives tempting researchers toward riskier work.
The true problem, one scientist suggested, lies not in India, but with a research system, rooted in the Global North, that has historically underwritten risky science.
Today, some experts said, because India’s high-containment laboratories are principally working to monitor pathogens that circulate in nature and on vaccine development, they pose less risk than facilities doing some other kinds of pathogen research. Labs such as NIHSAD, said Murugkar, are so overwhelmed with outbreak detection and response that they have little time or money for basic research and gain-of-function experiments. “It’s too much of hassle,” he said.
Anurag Agrawal, a researcher and dean at Ashoka University, echoed his point. “In India, there is not much manipulation going on of stuff that is unnatural,” he said, adding that Indian researchers are mostly occupied “collecting what exists in nature.”
The small scale of Indian biomedical research programs may preclude some of the ambitious experiments that result in pathogens acquiring pandemic potential, said immunologist Rath. Historically, American scientists have been able to create significantly more virulent and transmissible pathogens only after studying the microbes extensively, as part of long-running research programs. “I don’t think India has that level of large-scale research in any domain, in the life-sciences,” Rath said.
Agrawal recently served as a member of the Pathogens Project task force, an international consortium of researchers that sought to draw up basic guidelines for global biosafety, culminating in a presentation at the United Nations last year. Much of the risk, he suggested, comes through the involvement of international funders like the U.S. — which, in addition to shaping global biosafety policy, has also funded much, perhaps most, of the world’s higher-risk subset of gain-of-function research.
Under the government of Prime Minister Narendra Modi, it has become more difficult for India’s scientists to receive funding from government agencies outside of the country, including U.S. science agencies. One outcome of such policies, said Agrawal, is that laboratories and their staff aren’t under pressure to pursue riskier work in order to secure grant funding. “If people’s salaries depend on international grants, the pressure is high,” Agrawal said. “If the people’s salaries are assured by the government,” he added, “there is no pressure.”
* * *
Those kinds of assurances offer only partial comfort to biosafety experts. Intentional gain-of-function science is not the only kind of research that carries the risk of outbreaks. Sometimes, researchers can accidentally confer new abilities to pathogens. (In one notable incident, Australian researchers accidentally created a vaccine- and natural-immunity-resistant version of a mouse virus, a result one later described as “the kind of thing that science fiction is made of.”) And ordinary leaks of pathogens that are not widespread in the community can pose risks.
For now, no single organization oversees the expansion of pathogen research worldwide. The World Health Organization publishes influential recommendations on biosafety practice, but it lacks the power to determine whether countries are actually following them. “WHO has relatively few tools in its toolbox in terms of how it can be a global enforcement mechanism,” said Michaela Simoneau, an associate fellow at the Center for Strategic and International Studies.
In that void, a patchwork of initiatives has sprung up aiming to share knowledge across borders and develop global standards. Those collaborations focus on technical details, but also on intangible qualities such as laboratory culture that, some biosafety experts suggest, are just as crucial as Tyvek suits and ventilation systems. “The whole crux of this discussion is the culture that you establish within the laboratory,” said James Le Duc, who ran the Galveston National Laboratory in Texas, home to a major BSL-4 facility, until his retirement in 2022. (In recent writing, Le Duc and a colleague have argued that strong organizational-level leadership, not just “traditional top-down regulations,” is crucial for biosafety.)
“WHO has relatively few tools in its toolbox in terms of how it can be a global enforcement mechanism.”
Le Duc traveled to dozens of countries, including several trips to India, to work on laboratory development and build international collaborations. Until 2021, he also oversaw a program that allowed researchers from around the world to travel to Galveston and train in the BSL-4 laboratory there.
Getting money for those sorts of programs can be tough, Le Duc said: “There hasn’t been a source of funding to support this sort of collaboration. And that continues to be an issue.”
In India, scientists are sometimes distrustful of such outreach efforts, even if they think they may be useful. Murugkar said that American biosafety experts sometimes assume that India is rapidly expanding its lab network in secrecy, although things are different on the ground, where there is a shortage of labs and money. Most of the time, Americans compare India with China, he said, “but our situation and their situation is very different, because in a democratic setup, you can’t hide things.” And the excessive focus on biosecurity and engineered pathogens in American-run biosafety workshops, at a time when many Indian labs aren’t working on these, has made Indian researchers wary of such outreach, he said.
Americans, he added, “are a paranoid lot.”
There are also questions about how effective those collaborative programs are in preventing serious problems when they do arise. In the 2010s, Le Duc played an instrumental role in training scientists at the Wuhan Institute of Virology. His laboratory hosted a scientist from WIV for training in Texas, and he co-published papers on biosafety with the director of the Wuhan National Biosafety Laboratory.
Just weeks after the beginning of the COVID-19 pandemic, he wrote to that director with questions about safety there — and never heard back.
In light of the limits of such partnerships, what’s the value of the work? “I think the more that you work together,” Le Duc said, “the more opportunity that you have to share best practices, to answer questions as needed and to potentially avoid — and help others avoid — doing stupid things.”
* * *
For now, it’s hard to tell where the attempts to expand high-biocontainment research capacity in India will end up.
Previous attempts have often hit roadblocks, and Murugkar said funding is a problem at many government labs: Money to build the lab is relatively easy to come by, but maintenance funds are harder to secure. When labs remain underutilized between outbreaks, policymakers tend to question whether the expense is worth it.
Hindrances can also be political. The Indian government’s wariness for American collaborations has sometimes led it to shut down research — whether or not that’s warranted. In 2020, for example, the Hindu, a major Indian daily news outlet, reported that the Indian Council of Medical Research, a government medical research agency, had accused another scientific agency of breaching biosafety protocols while doing research on bat-borne pathogens in northeastern India. Internal documents viewed by Undark revealed that part of the concern arose from the fact that the research was funded by the U.S. Department of Defense. Eventually, the group was cleared of the charges, and allowed to resume its work, but stayed away from U.S. funding.
The accusations had a freezing effect on other groups studying bat viruses, according to one researcher familiar with the dispute, who requested anonymity in order to avoid jeopardizing future work.
Uncertainty around their role in outbreak responses has made some institutions rethink their plans to build high biocontainment labs. Among them is the Rajiv Gandhi Center for Biotechnology, which received a greenlight from the central government to build a BSL-4 lab in 2020. Four years later, though, Narayana, its director, said they have dropped the idea. The worry, he said, is that the India Council for Medical Research (ICMR), which coordinates research into outbreaks across the country, may not include their lab in outbreak responses, and the expensive facility they develop would remain under-used. (ICMR did not respond to a request for comment.)

Schwartz, the Indian American biosafety expert, also expressed concern about biosafety and regulations of biological research coming to be seen as a roadblock. Speaking on Zoom recently, Schwartz evoked a dynamic that has emerged in conversations about climate change. Wealthy countries, he noted, used fossil fuels to make advancements — and now are turning around and telling less wealthy countries to stop emitting greenhouse gases. The perception, he said, is you made advancements “and now you’re trying to slow us down.”
The same, Schwartz suggested, could apply to biosafety. Wealthy countries developed their own pathogen research programs during an era of far less attention and global scrutiny. A shortage of high containment facilities made it difficult for India and other countries in the Global South to respond to the virus. Would biosafety restrictions be seen as a valuable tool for public safety, or as another way of hampering progress?
“You don’t want biosafety to be seen as a stumbling block or seen as a way to slow things down,” Schwartz said.
Murugkar said that finding the balance between high biosafety standards and continuing to do critical diagnostic work is hard in a country like India. Thrusting “absolute American standards” on Indian diagnostic labs, already struggling with the lack of resources, would stop important public health work, Murugkar said. On the other hand, poor biosafety hurts public health too. It’s a challenging trade-off, he said. “Where do you draw a line?”
Your support is crucial...As we navigate an uncertain 2025, with a new administration questioning press freedoms, the risks are clear: our ability to report freely is under threat.
Your tax-deductible donation enables us to dig deeper, delivering fearless investigative reporting and analysis that exposes the reality beneath the headlines — without compromise.
Now is the time to take action. Stand with our courageous journalists. Donate today to protect a free press, uphold democracy and uncover the stories that need to be told.

You need to be a supporter to comment.
There are currently no responses to this article.
Be the first to respond.